Healthcare Member Benefit – Program Background

Program Background:
- This is an exclusive Member Benefit Program available to members of Gig Workers Universe across the country.
- This Program is not available through health insurance brokers, is not available commercially or on the federal marketplace.
- GWU Members who wish to access these Member Benefits (which include Health, Rx and supplemental plans) can do this by becoming and Associate Member of Local 426.
- As an Associate Member of Amalgamated Local 426, you do not have collective bargaining, voting or striking rights.
- This is truly a vehicle that allows you to access these specific Member Benefits.
How Does it Work?
- The Sponsoring Union (Local 298) is a Taft-Hartley, self-insured Health and Welfare Benefits Plan with over 10,000 participants
- Local 298 takes the risk on behalf of all enrolled participants, including Local 426 participants
- Local 298 provides Amalgamated Local 426 with rates each year.
- The program uses a four-tier rate structure (EE, EECH, EESP, EEFAM)
- Rates are not based on factors like age/gender, medical underwriting and does not apply preexisting conditions
- Benefit Program renewal rates are based on the total plan participants experience
- All participants receive the same increase regardless of individual claims
- As a self-insured program, Local 298 processed their own claims and contracts with all the vendors including the network, pharmacy vendor and third-party administrators.

Plan Options
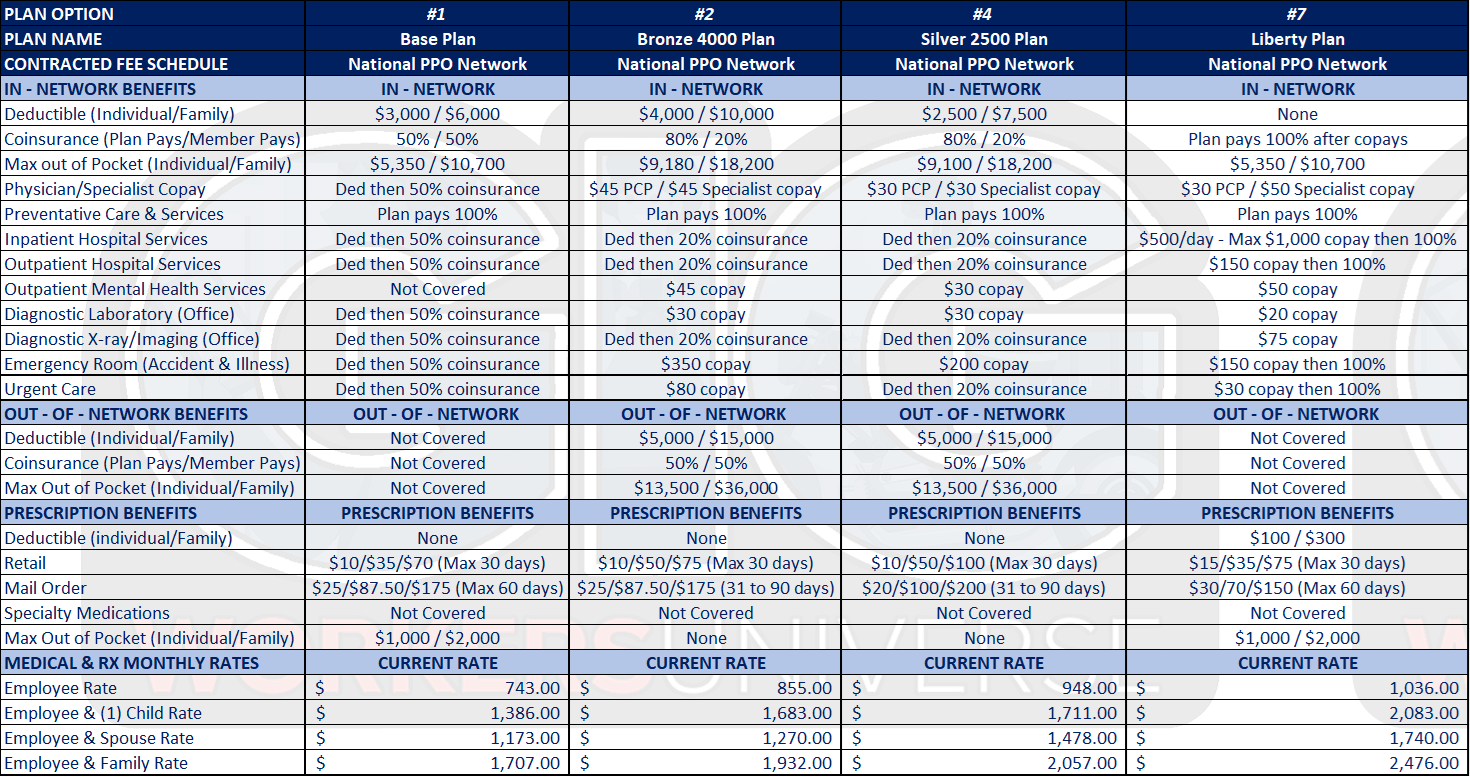
Healthcare Member Benefit Program
Important Benefit and Plan Information

Benefit Designs:
Plan designs are static and cannot be changed or revised.

Rates:
The current rates are effective 7/1/2023 through 6/30/2024. Groups with an initial effective date of 7/1, 8/1, 9/1, 10/1, 11/1 and 12/1 will renew July 1st each year following. Groups with an initial effective date of 1/1, 2/1, 3/1, 4/1, 5/1 and 6/1 will renew January 1st each year following.

Specialty Drug Coverage:
Prior Authorization Required under Payer Matrix Program. Effective as of January 1, 2018, the Plan will offer specialty drugs (including non-multisource chemotherapy prescription drugs) only if approved and provided through Payer Matrix Program. As such, all participants are required to meet the prior authorization criteria and administrative review under this program. This pre-authorization requirement will also apply to all self-injectable prescribed drugs, home infusion medications, chemotherapy prescribed drugs and injectables given at a provider’s office or a network facility. Accordingly, to be eligible for specialty drugs, you must enroll in the Payer Matrix program, or you will be responsible for 100% co-insurance or the full cost of the medication.

Automobile Accident Coverage
It is especially important to understand that this Plan will not pay for any expenses incurred as the result of a motor vehicle accident. Lately, it has become popular for States to attempt to transfer the automobile carrier’s liability over to the employee’s medical plan. While it is true this may result in the saving of a few premium dollars for the automobile insurance carrier, it exposes your employer’s benefit plan to extremely large and possibly ruinous losses; losses it was never intended to cover. It is your obligation to purchase adequate medical coverage in your automobile insurance plan to assure your coverage is sufficient. (See next page for additional accident coverage).




